Cochlear nerve inflammation, also known as cochlear neuritis, is a medical condition that affects the cochlear nerve, a crucial component of our auditory system. This condition can lead to various hearing problems, including hearing loss and tinnitus. Understanding the intricacies of the cochlear nerve, the science behind its inflammation, the symptoms, diagnosis, treatment options, and prevention techniques is vital in managing this condition effectively.
Understanding the Cochlear Nerve
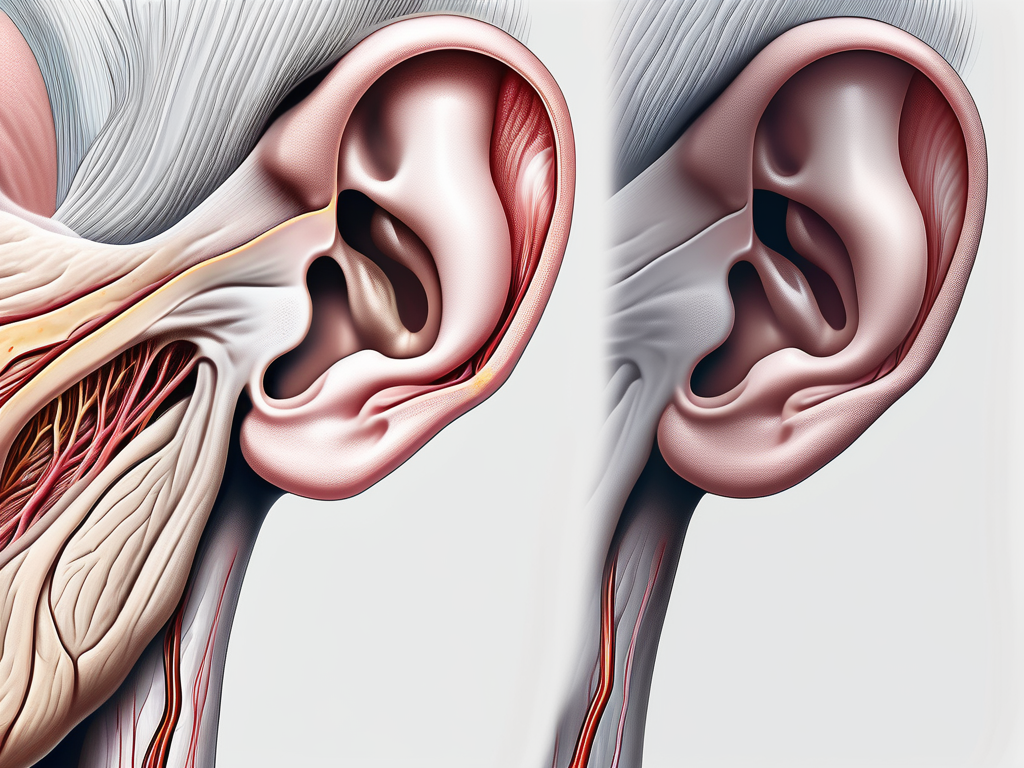
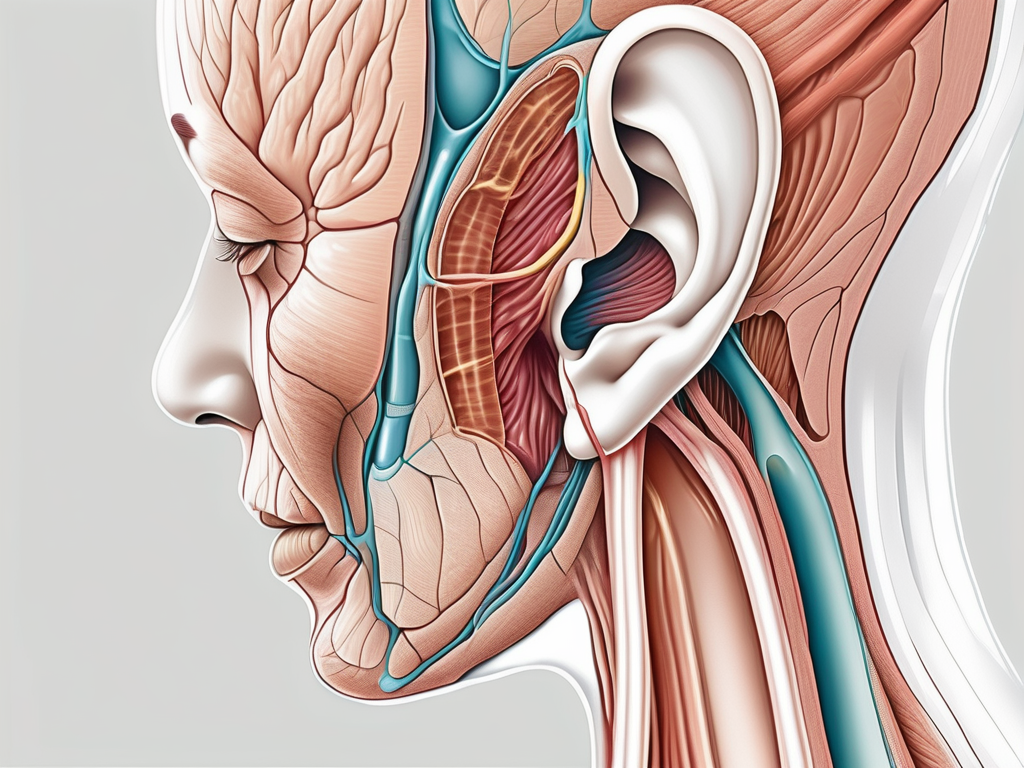
Before delving into the complexities of cochlear nerve inflammation, it is important to grasp the basic anatomy and function of the cochlear nerve. The cochlear nerve is a branch of the vestibulocochlear nerve (also known as cranial nerve VIII) and is responsible for transmitting auditory signals from the cochlea to the brain. This allows us to perceive sound and interpret it accordingly.
The cochlear nerve, although small in size, plays a crucial role in our auditory system. Let’s explore its anatomy and function in more detail.
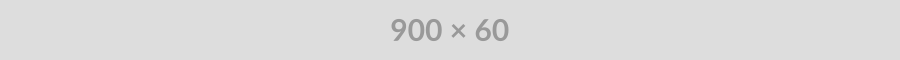
Anatomy of the Cochlear Nerve
The cochlear nerve is composed of thousands of small nerve fibers that bundle together to form the auditory nerve. These fibers are essential for the transmission of electrical signals between the cochlea and the brain. Without these intricate fibers, our ability to hear and comprehend sound would be severely compromised.
The journey of these nerve fibers begins in the cochlea, a spiral-shaped structure located in the inner ear. Within the cochlea, there are specialized sensory cells called hair cells. These hair cells convert sound vibrations into electrical signals, which are then picked up by the nerve fibers of the cochlear nerve.
As the nerve fibers exit the cochlea, they form a compact bundle that travels through the bony structures of the inner ear. This bundle, known as the cochlear nerve, carries the electrical signals towards the brain for further processing and interpretation.
Upon reaching the brain, the cochlear nerve fibers connect with the auditory processing centers, such as the auditory cortex. These centers are responsible for analyzing the electrical signals and translating them into meaningful sounds that we can perceive and understand.
Function of the Cochlear Nerve
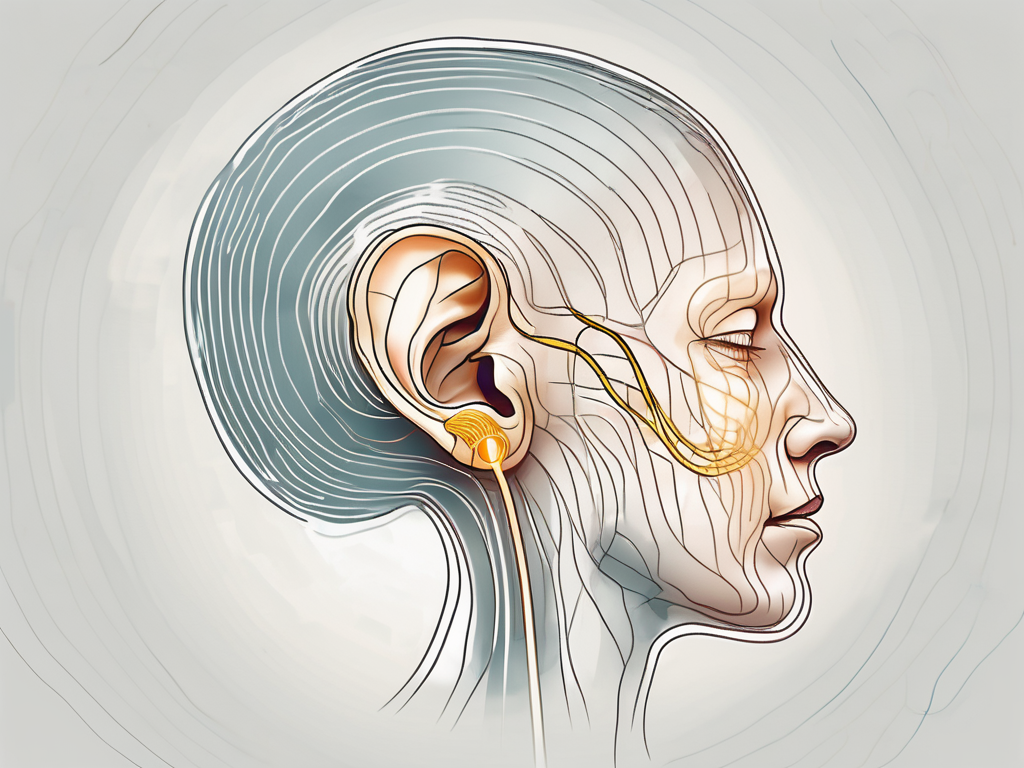
The primary function of the cochlear nerve is to transmit auditory information from the cochlea to the brain. This involves converting sound vibrations captured by the cochlea into electrical signals that can be understood by the brain. By serving as the intermediary between the ear and the brain, the cochlear nerve plays a vital role in our ability to hear and interpret sound accurately.
When sound waves enter the ear, they cause the hair cells in the cochlea to vibrate. These vibrations are then translated into electrical signals, which are picked up by the nerve fibers of the cochlear nerve. These signals are then relayed to the brain, where they are processed and interpreted as different sounds.
It is important to note that the cochlear nerve is not only responsible for transmitting sound signals but also plays a role in distinguishing different frequencies and volumes of sound. This allows us to perceive a wide range of sounds, from the softest whispers to the loudest explosions.
Furthermore, the cochlear nerve is capable of adapting to different sound environments. It can adjust its sensitivity to ensure that we can hear sounds clearly, even in noisy or challenging situations. This remarkable ability of the cochlear nerve enables us to communicate effectively and engage with the world around us.
In conclusion, the cochlear nerve is a remarkable component of our auditory system. Its intricate anatomy and vital function make it an essential part of our ability to hear and interpret sound. Understanding the complexities of the cochlear nerve helps us appreciate the incredible mechanisms that allow us to experience the richness of the auditory world.
The Science Behind Cochlear Nerve Inflammation
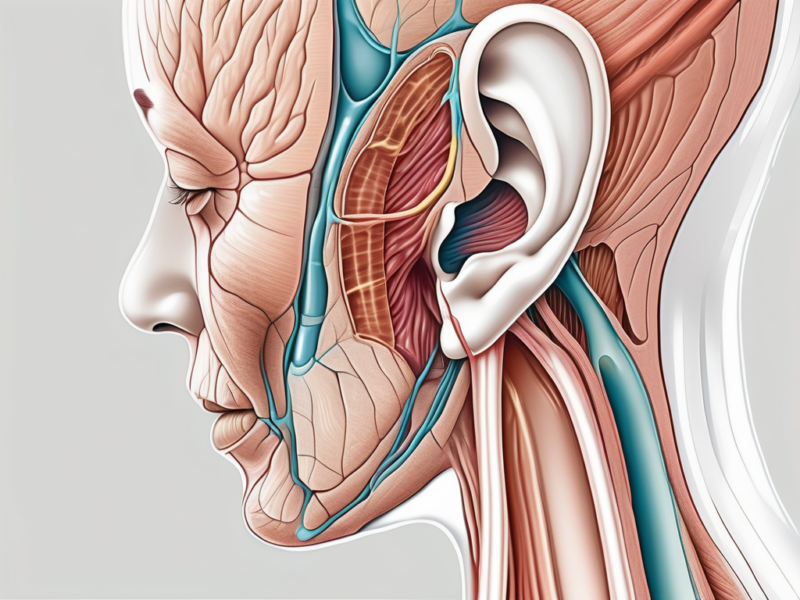
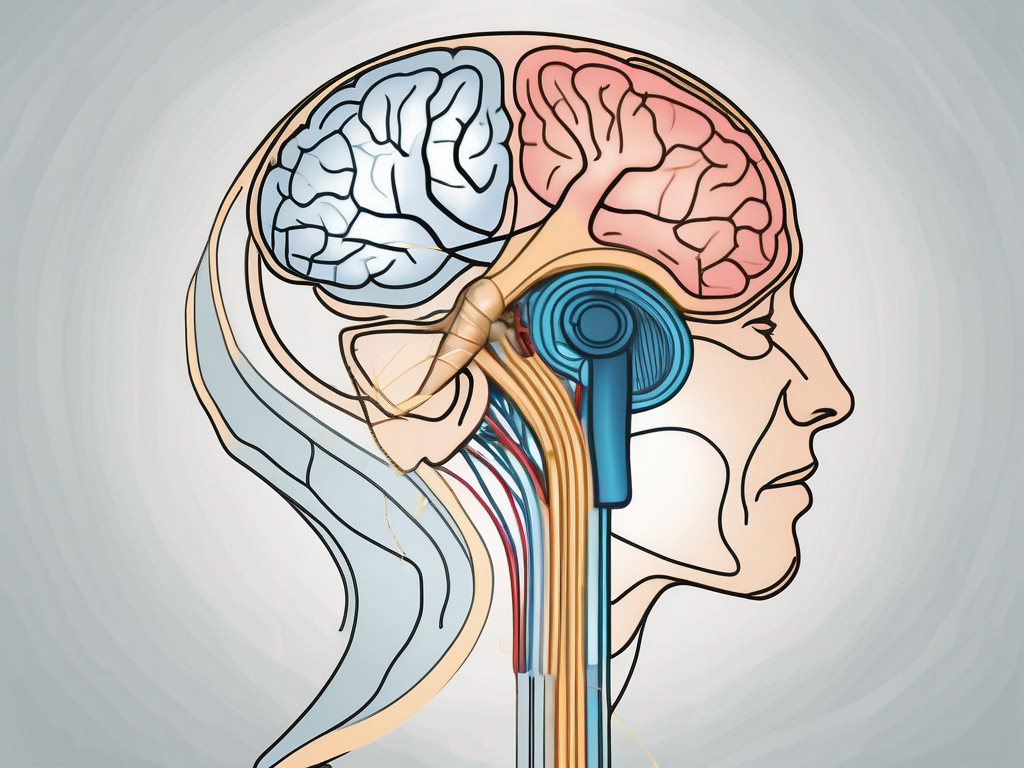
Cochlear nerve inflammation occurs when the nerve becomes swollen or irritated. This inflammation disrupts the normal transmission of auditory signals between the cochlea and the brain, leading to a range of auditory problems. Understanding the causes and pathophysiology of cochlear nerve inflammation is essential for effective diagnosis and treatment.
The cochlear nerve, also known as the auditory nerve, is a crucial component of the auditory system. It is responsible for transmitting sound information from the cochlea, a spiral-shaped structure in the inner ear, to the brain. When this nerve becomes inflamed, the intricate process of converting sound waves into electrical signals and transmitting them to the brain is disrupted.
Causes of Cochlear Nerve Inflammation
There are several potential causes of cochlear nerve inflammation, each with its own unique set of factors and implications. Viral infections, such as mumps, measles, and influenza, have been known to trigger inflammation in the cochlear nerve. These infections can directly affect the nerve or stimulate an immune response that leads to inflammation.
Autoimmune disorders, like multiple sclerosis, can also cause cochlear nerve inflammation. In these conditions, the body’s immune system mistakenly attacks and damages the nerve, leading to inflammation and subsequent auditory problems. The exact mechanisms behind the immune system’s involvement in cochlear nerve inflammation are still being studied.
Furthermore, certain medications have been linked to cochlear nerve inflammation. Ototoxic drugs, which are known to have toxic effects on the ear, can contribute to inflammation in the cochlear nerve. Some antibiotics and chemotherapy drugs fall into this category and may have unintended consequences on the auditory system.
Pathophysiology of Cochlear Nerve Inflammation
When the cochlear nerve becomes inflamed, the delicate balance of electrical signals between the cochlea and the brain is disturbed. This disruption in signal transmission leads to various auditory symptoms, including hearing loss, tinnitus (ringing in the ears), and difficulties in speech perception.
The exact mechanisms behind cochlear nerve inflammation are still under investigation. However, researchers believe that the immune system’s response plays a significant role in causing the inflammation. In response to viral infections or autoimmune disorders, the immune system releases inflammatory molecules that can affect the nerve’s function and structure.
Additionally, the release of pro-inflammatory cytokines, which are signaling molecules involved in immune responses, may contribute to the development of cochlear nerve inflammation. These cytokines can promote the recruitment of immune cells to the site of inflammation, leading to further damage and disruption of auditory signal transmission.
Moreover, oxidative stress, a condition characterized by an imbalance between antioxidants and harmful reactive oxygen species, has been implicated in cochlear nerve inflammation. The production of reactive oxygen species can damage the nerve cells and trigger an inflammatory response.
Overall, understanding the causes and pathophysiology of cochlear nerve inflammation is crucial for developing effective diagnostic methods and targeted treatments. By unraveling the complex mechanisms behind this condition, researchers and healthcare professionals can work towards improving the quality of life for individuals affected by auditory problems associated with cochlear nerve inflammation.
Symptoms and Diagnosis of Cochlear Nerve Inflammation
Recognizing the symptoms of cochlear nerve inflammation is crucial for early detection and appropriate medical intervention. While it is essential to consult with a medical professional for an accurate diagnosis, being aware of the common symptoms can help prompt timely medical attention.
Cochlear nerve inflammation, also known as cochlear neuritis, occurs when the nerve responsible for transmitting sound signals from the inner ear to the brain becomes inflamed. This inflammation can disrupt the normal functioning of the nerve, leading to various symptoms that can significantly impact a person’s quality of life.
Recognizing the Symptoms
The symptoms of cochlear nerve inflammation can vary from person to person, but often include sudden hearing loss, tinnitus (ringing in the ears), dizziness, and imbalance. Some individuals may also experience ear pain or pressure, as well as difficulty understanding speech in noisy environments.
Sudden hearing loss is one of the hallmark symptoms of cochlear nerve inflammation. It can occur in one or both ears and may be accompanied by a feeling of fullness or pressure in the affected ear. Tinnitus, another common symptom, can manifest as a persistent ringing, buzzing, or hissing sound in the ears. This phantom noise can be disruptive and distressing, making it difficult for individuals to concentrate or sleep.
Dizziness and imbalance are also prevalent symptoms of cochlear nerve inflammation. These symptoms can make it challenging to maintain stability and can increase the risk of falls. The sensation of dizziness may be accompanied by a spinning or lightheaded feeling, further impacting a person’s ability to perform daily activities.
Diagnostic Procedures
To diagnose cochlear nerve inflammation, a medical professional will conduct various tests such as audiological evaluations, including pure-tone audiometry and speech audiometry. These tests help assess the severity and extent of hearing loss. Pure-tone audiometry involves wearing headphones and listening to tones at different frequencies and volumes. The individual indicates when they can hear the tones, allowing the healthcare provider to determine the degree of hearing loss.
Speech audiometry, on the other hand, evaluates a person’s ability to understand and repeat words or sentences at different volumes. This test helps determine if the inflammation is affecting the individual’s ability to comprehend speech, especially in noisy environments.
In addition to audiological evaluations, imaging techniques like magnetic resonance imaging (MRI) can provide detailed images of the inner ear, aiding in the diagnosis of cochlear nerve inflammation and ruling out other possible causes. An MRI can help identify any structural abnormalities or signs of inflammation in the cochlea and surrounding structures.
Early diagnosis of cochlear nerve inflammation is crucial to prevent further damage and initiate appropriate treatment. If you experience any of the symptoms mentioned, it is important to seek medical attention promptly. Remember, only a healthcare professional can provide an accurate diagnosis and recommend the most suitable treatment options.
Treatment Options for Cochlear Nerve Inflammation
When it comes to treating cochlear nerve inflammation, the specific approach depends on the underlying cause, severity of symptoms, and the individual’s overall health. It is crucial to consult with an ear, nose, and throat specialist or an audiologist for a comprehensive evaluation and personalized treatment plan.
Cochlear nerve inflammation, also known as cochlear neuritis, can be a debilitating condition that affects the auditory nerve, leading to hearing loss and other related symptoms. The inflammation can be caused by various factors, including viral infections, autoimmune disorders, and even certain medications. Understanding the underlying cause is essential in determining the most effective treatment options.
Medication and Therapy
In cases where viral infections or autoimmune disorders are responsible for cochlear nerve inflammation, antiviral medication or immunosuppressants may be prescribed to treat the underlying condition and reduce inflammation. These medications work by targeting the specific cause of the inflammation, helping to alleviate symptoms and prevent further damage to the auditory nerve.
Furthermore, therapy can play a crucial role in the treatment of cochlear nerve inflammation. Physical therapy and vestibular rehabilitation exercises can help improve balance and reduce dizziness, which are common symptoms associated with this condition. Speech therapy may also be recommended to help individuals cope with any hearing loss and improve communication abilities.
For individuals experiencing significant hearing loss as a result of cochlear nerve inflammation, hearing aids and cochlear implants may be recommended. Hearing aids amplify sounds, making them louder and clearer, while cochlear implants bypass the damaged auditory nerve and directly stimulate the cochlea, allowing individuals to perceive sound signals.
Surgical Interventions
In some cases, surgical interventions may be necessary to alleviate the symptoms of cochlear nerve inflammation. This may include surgeries to drain fluid from the inner ear, repair damaged structures, or implant neurostimulation devices that bypass the affected nerve fibers and directly stimulate the cochlea or auditory nerve.
One surgical option is a cochlear implant, which is a small electronic device that is surgically implanted into the inner ear. It works by converting sound into electrical signals that directly stimulate the auditory nerve, bypassing the damaged cochlear nerve fibers. Cochlear implants have been proven to be highly effective in restoring hearing in individuals with severe to profound hearing loss.
In cases where the inflammation is caused by a buildup of fluid in the inner ear, a surgical procedure called a tympanostomy may be performed. This procedure involves making a small incision in the eardrum to drain the fluid and relieve pressure, helping to reduce inflammation and improve hearing.
Another surgical option is the implantation of a neurostimulation device, such as a cochlear nerve stimulator or an auditory brainstem implant. These devices work by directly stimulating the auditory nerve or the brainstem, bypassing the damaged cochlear nerve fibers and allowing individuals to perceive sound signals.
It is important to note that the decision to undergo surgical intervention for cochlear nerve inflammation is not taken lightly. The risks, benefits, and potential outcomes of each procedure should be thoroughly discussed with a healthcare professional to determine the most suitable course of action.
In conclusion, the treatment options for cochlear nerve inflammation are diverse and depend on various factors. Medication, therapy, and surgical interventions can all play a role in managing the symptoms and improving the quality of life for individuals affected by this condition. Consulting with a healthcare professional is crucial in developing a personalized treatment plan that addresses the specific needs and circumstances of each individual.
Living with Cochlear Nerve Inflammation
Living with cochlear nerve inflammation can present unique challenges. However, there are coping mechanisms and strategies that can help individuals manage their symptoms and improve their quality of life.
When living with cochlear nerve inflammation, it is important to understand the impact it can have on various aspects of life. For instance, individuals may experience difficulties in social situations, as hearing conversations and understanding speech can become challenging. This can lead to feelings of isolation and frustration. However, by seeking emotional support from friends, family, and support groups, individuals can find solace and understanding. Sharing experiences with others who are going through similar challenges can provide a sense of community and help individuals feel less alone in their journey.
In addition to emotional support, exploring assistive listening devices and communication techniques can significantly improve communication abilities. For example, using hearing aids or cochlear implants can enhance sound perception and clarity. These devices work by amplifying sounds and transmitting them directly to the inner ear, bypassing the damaged cochlear nerve. Furthermore, learning communication strategies, such as lip-reading or sign language, can also be beneficial in overcoming communication barriers.
Living with cochlear nerve inflammation can be stressful, both physically and emotionally. Therefore, practicing stress management techniques is crucial. Engaging in activities like meditation and relaxation exercises can help individuals reduce anxiety and promote a sense of calm. These techniques can also aid in coping with the emotional impact of the condition, allowing individuals to maintain a positive outlook and improve their overall well-being.
Long-Term Prognosis and Management
The long-term prognosis for individuals with cochlear nerve inflammation varies depending on the underlying cause, severity of symptoms, and individual factors. It is important to work closely with medical professionals to develop an ongoing management plan that includes regular check-ups and monitoring of symptoms.
Regular check-ups are essential for tracking the progression of the condition and ensuring that appropriate interventions are in place. Medical professionals may conduct various tests, such as audiograms and imaging scans, to assess the extent of nerve inflammation and monitor any changes over time. By closely monitoring the condition, healthcare providers can make informed decisions regarding treatment options and adjustments to the management plan.
Following recommended treatment regimens is crucial in effectively managing cochlear nerve inflammation. Treatment options may include medications to reduce inflammation, physical therapy to improve balance and coordination, or surgical interventions in severe cases. It is important to adhere to the prescribed treatment plan and communicate any concerns or side effects to the healthcare team.
In addition to medical interventions, making necessary lifestyle adjustments can also help individuals effectively manage their condition and minimize its impact on their daily lives. For instance, taking steps to protect the ears from loud noises, such as wearing earplugs or avoiding noisy environments, can prevent further damage to the cochlear nerve. Additionally, maintaining a healthy lifestyle by eating a balanced diet, exercising regularly, and getting enough sleep can contribute to overall well-being.
Living with cochlear nerve inflammation may pose challenges, but with the right support, coping mechanisms, and management strategies, individuals can lead fulfilling lives. By staying proactive in their care and seeking assistance when needed, individuals can navigate the complexities of this condition and continue to thrive.
Prevention of Cochlear Nerve Inflammation
While it may not always be possible to prevent cochlear nerve inflammation, some lifestyle changes and proactive measures can reduce the risk of developing this condition.
Lifestyle Changes
Avoiding exposure to loud noises, wearing ear protection in noisy environments, and practicing good ear hygiene, such as gentle cleaning and avoiding the use of cotton swabs, can help reduce the risk of developing cochlear nerve inflammation. It is also important to prioritize overall health and well-being by maintaining a balanced diet, engaging in regular exercise, and managing stress levels effectively.
Regular Check-ups and Early Detection
Regular check-ups with an audiologist or otolaryngologist (ear, nose, and throat specialist) are crucial for early detection and intervention in cases of cochlear nerve inflammation. These professionals can monitor hearing health, provide personalized recommendations, and detect any changes in auditory function promptly.
In conclusion, cochlear nerve inflammation is a complex condition that affects the auditory system. By understanding its anatomy, causes, diagnosis, treatment options, and prevention techniques, individuals can work with medical professionals to effectively manage this condition and improve their quality of life. If you suspect any auditory difficulties or symptoms related to cochlear nerve inflammation, it is important to consult with a medical professional for appropriate evaluation and guidance.